VA System Rolls Out 3D Printing
VA System Rolls Out 3D Printing
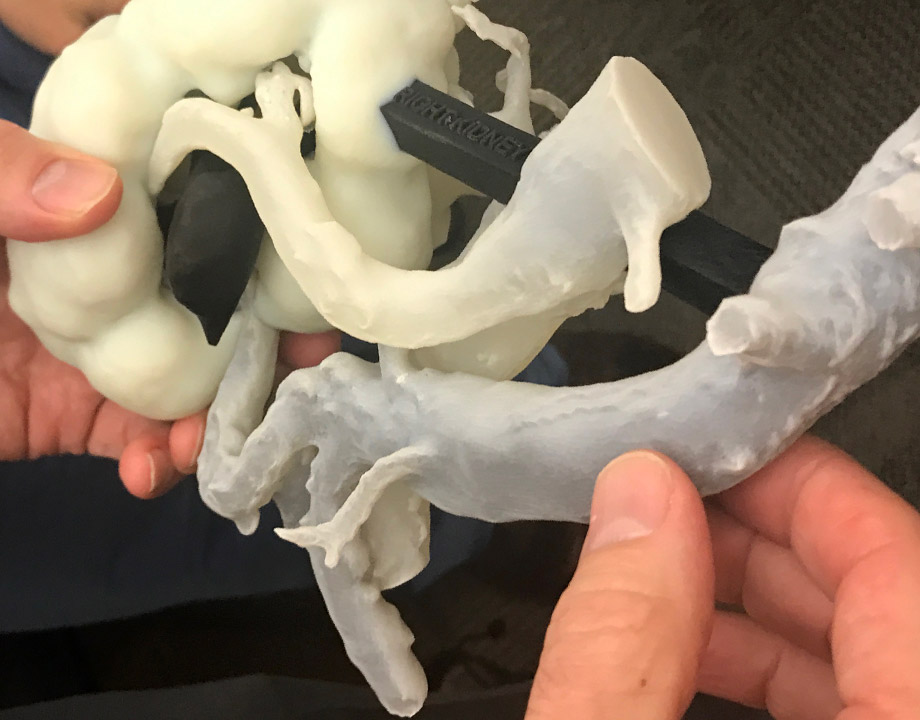
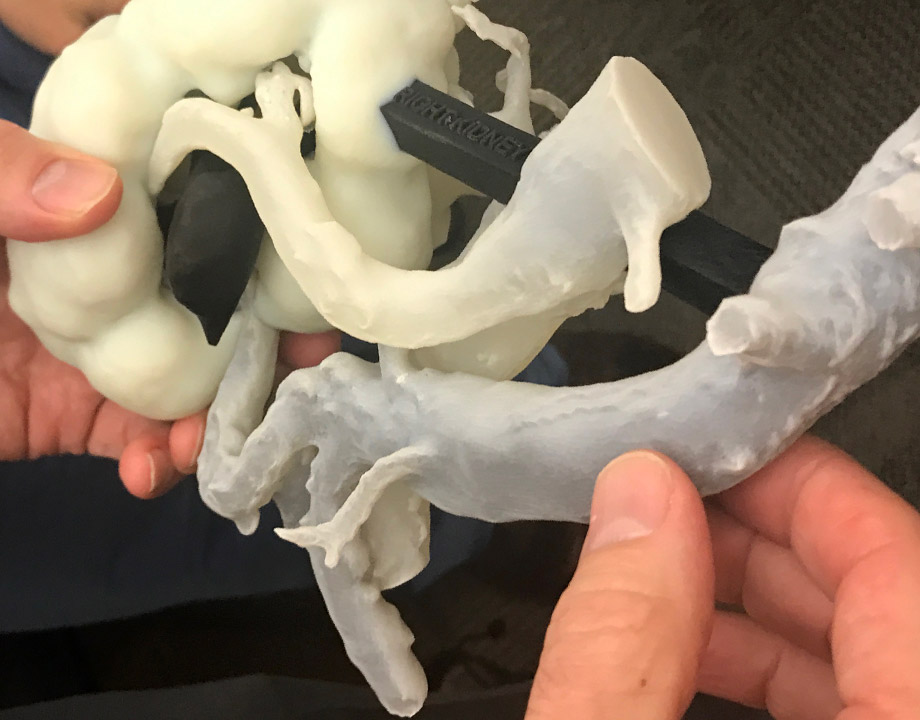
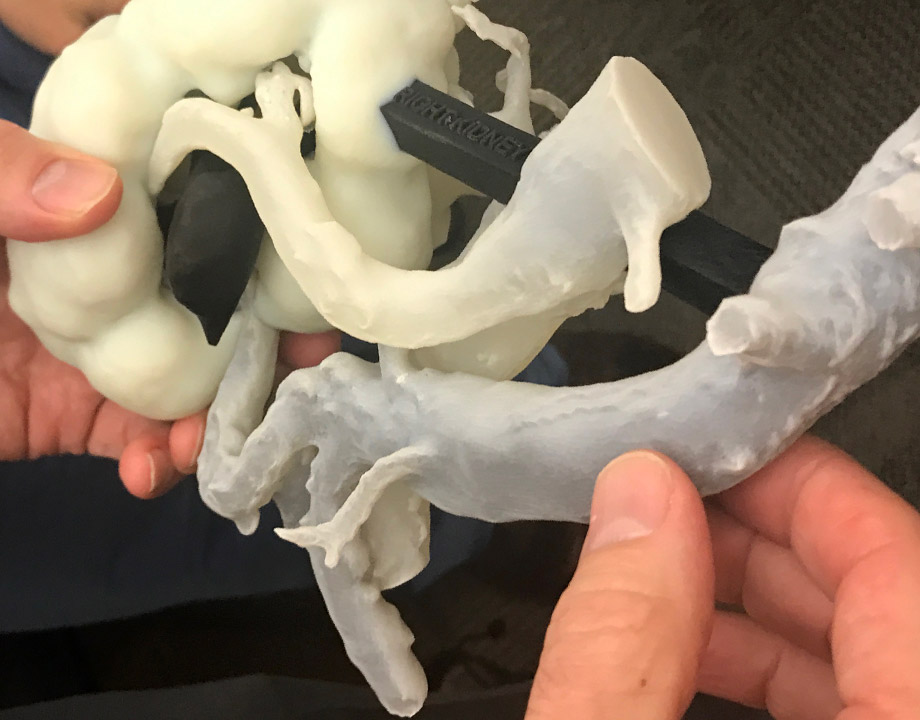
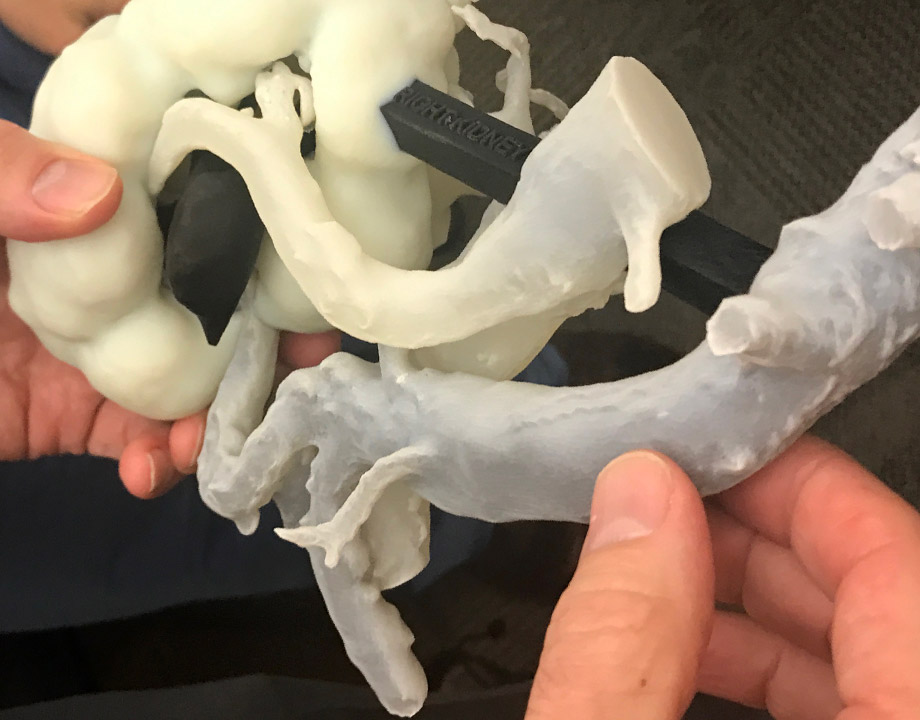
VA is exploring ways in which 3D printing can solve a wide range of problems, such as pre-surgical planning. Photo: VA Puget Sound
With 170 medical centers and 1,063 outpatient facilities, the U.S. Department of Veterans Affairs is the nation’s largest integrated health care system. The VA currently uses 3D printing at several of its hospitals, and plans to begin rolling it out at all its hospitals over the next couple of years.
Dr. Beth Ripley, a radiologist at the VA Puget Sound Healthcare System in Seattle, is leading the project. She explains how she uses the technology in her hospital and how she plans to roll out 3D printing throughout the VA system.
Q: How do you use 3D printing at VA Puget Sound?
B.R: VA Puget Sound is our flagship hospital for pre-surgical planning. We have been working with surgeons, engineers, and IT staff to build a program that allows us to provide surgeons with exact replicas of each individual patient’s anatomy. The 3D-printed model helps surgeons understand the case better. It also helps the patient understand the problem better.
Q: How is this different from skeleton models in doctors’ offices?
B.R: Those models give you a general idea [of what something looks like], but it’s not you. We’re trying to really understand your anatomy, not an artist’s version or something generic. Those small details that make your anatomy yours are also what make cases challenging. Understanding that difference makes your treatment that much better.
For example, we recently had a patient who was born with a single kidney. We were able to 3D print that patient’s anatomy within submillimeter resolution and accuracy.
Further Reading: 3D Printing Overcoming Biocompatibility Challenge
Q: What did you use that model for? Was it for a kidney surgery?
B.R: Yes, the patient had developed a tumor on the kidney. Since he had only one kidney, we couldn’t take the kidney out or he’d be on dialysis for the rest of his life. So, the surgeon was trying to understand how he could remove just the portion that had the tumor.
The surgeon was able to look at the 3D-printed model, think about all the potential complications, the best way to approach the surgery, where to cut, and rehearse all of that before operating.
Q: Given all the different uses for 3D printing, why was this your first implementation of the technology?
B.R: It’s totally driven by the interest of the frontline staff at the hospital. I happen to be a radiologist, so I look at medical imaging every day. 3D printing allows me to do my job better by being able to take those complicated images and translate them into these tangible models. So we focused on that.
We have a hospital in New Orleans where the 3D printer landed in the prosthetics department. They’re using it to make better prosthetics. We have, by design, placed 3D printers into the hands of frontline staff that have real problems they’re trying to solve. As they come up with new solutions, we share those solutions and scale up.
Q: How many VA hospitals have 3D printers?
B.R: Back in 2017, there were three hospitals that were already printing for three or four years. At the end of 2017, we put printers into five more hospitals. We’ve now grown to 33 hospitals, and a lot of this work is coming out of the VA innovation ecosystem.
Q: Did you meet with resistance early on?
B.R: Definitely. It’s really hard to forecast how helpful and impactful any new technology will be, especially in a hospital setting where we value quality, safety, and high reliability. So, necessarily, people are skeptical of new technology.
We were really thoughtful about how we rolled it out. In the initial innovation phase, we tested it in a very structured and contained way, so we knew how it was going to impact our patients before we opened the floodgates. We didn’t place it into clinical practice until we were able to see the benefits and verify that it was safe. We developed regulations and checkpoints to make sure that we’re using the same [protocols] across the organization.
Further Reading: 3D Printing Medical Scans
Q: What's next and how will you roll out 3D printing across the whole VA system?
B.R: Our goal for 3D printing across the VA is to figure out the sweet spot to provide care for all nine million veterans while maximizing resources. We’re trying to understand how many printers we need. How many personnel? How can we link them together to make sure we can treat all of our patients regardless of whether there is a 3D printer at their home hospital?
In a year or two we might be able to 3D print actual implants using titanium metal printers. We’re exploring bio-printing too. Instead of printing something metal can we replace part of the bone by bioprinting a piece of bone or cartilage?
Poornima Apte is an engineering writer based in Boston.
Register Today for AM Medical: May 27–28, 2020 in Minneapolis, MN
Dr. Beth Ripley, a radiologist at the VA Puget Sound Healthcare System in Seattle, is leading the project. She explains how she uses the technology in her hospital and how she plans to roll out 3D printing throughout the VA system.
Q: How do you use 3D printing at VA Puget Sound?
B.R: VA Puget Sound is our flagship hospital for pre-surgical planning. We have been working with surgeons, engineers, and IT staff to build a program that allows us to provide surgeons with exact replicas of each individual patient’s anatomy. The 3D-printed model helps surgeons understand the case better. It also helps the patient understand the problem better.
Q: How is this different from skeleton models in doctors’ offices?
B.R: Those models give you a general idea [of what something looks like], but it’s not you. We’re trying to really understand your anatomy, not an artist’s version or something generic. Those small details that make your anatomy yours are also what make cases challenging. Understanding that difference makes your treatment that much better.
For example, we recently had a patient who was born with a single kidney. We were able to 3D print that patient’s anatomy within submillimeter resolution and accuracy.
Further Reading: 3D Printing Overcoming Biocompatibility Challenge
Q: What did you use that model for? Was it for a kidney surgery?
B.R: Yes, the patient had developed a tumor on the kidney. Since he had only one kidney, we couldn’t take the kidney out or he’d be on dialysis for the rest of his life. So, the surgeon was trying to understand how he could remove just the portion that had the tumor.
The surgeon was able to look at the 3D-printed model, think about all the potential complications, the best way to approach the surgery, where to cut, and rehearse all of that before operating.
Q: Given all the different uses for 3D printing, why was this your first implementation of the technology?
B.R: It’s totally driven by the interest of the frontline staff at the hospital. I happen to be a radiologist, so I look at medical imaging every day. 3D printing allows me to do my job better by being able to take those complicated images and translate them into these tangible models. So we focused on that.
We have a hospital in New Orleans where the 3D printer landed in the prosthetics department. They’re using it to make better prosthetics. We have, by design, placed 3D printers into the hands of frontline staff that have real problems they’re trying to solve. As they come up with new solutions, we share those solutions and scale up.
Q: How many VA hospitals have 3D printers?
B.R: Back in 2017, there were three hospitals that were already printing for three or four years. At the end of 2017, we put printers into five more hospitals. We’ve now grown to 33 hospitals, and a lot of this work is coming out of the VA innovation ecosystem.
Q: Did you meet with resistance early on?
B.R: Definitely. It’s really hard to forecast how helpful and impactful any new technology will be, especially in a hospital setting where we value quality, safety, and high reliability. So, necessarily, people are skeptical of new technology.
We were really thoughtful about how we rolled it out. In the initial innovation phase, we tested it in a very structured and contained way, so we knew how it was going to impact our patients before we opened the floodgates. We didn’t place it into clinical practice until we were able to see the benefits and verify that it was safe. We developed regulations and checkpoints to make sure that we’re using the same [protocols] across the organization.
Further Reading: 3D Printing Medical Scans
Q: What's next and how will you roll out 3D printing across the whole VA system?
B.R: Our goal for 3D printing across the VA is to figure out the sweet spot to provide care for all nine million veterans while maximizing resources. We’re trying to understand how many printers we need. How many personnel? How can we link them together to make sure we can treat all of our patients regardless of whether there is a 3D printer at their home hospital?
In a year or two we might be able to 3D print actual implants using titanium metal printers. We’re exploring bio-printing too. Instead of printing something metal can we replace part of the bone by bioprinting a piece of bone or cartilage?
Poornima Apte is an engineering writer based in Boston.
Register Today for AM Medical: May 27–28, 2020 in Minneapolis, MN